Brain Tumor survivors now a Physician Assistant and Registered Nurse promote brain tumor awareness during May Brain Tumor Awareness Month. Both clinicians work in Addiction Medicine, providing primary care to patients undergoing detoxification and both are survivors of a brain tumor diagnosis and treatment.
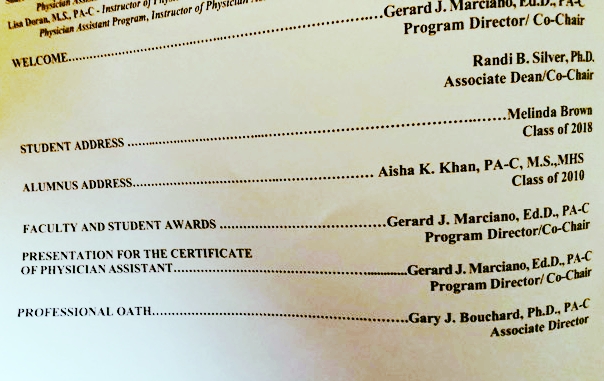
Read moreInvited as Guest Speaker for Weill Cornell Medical College Physician Assistant Program Graduation White Coat Ceremony
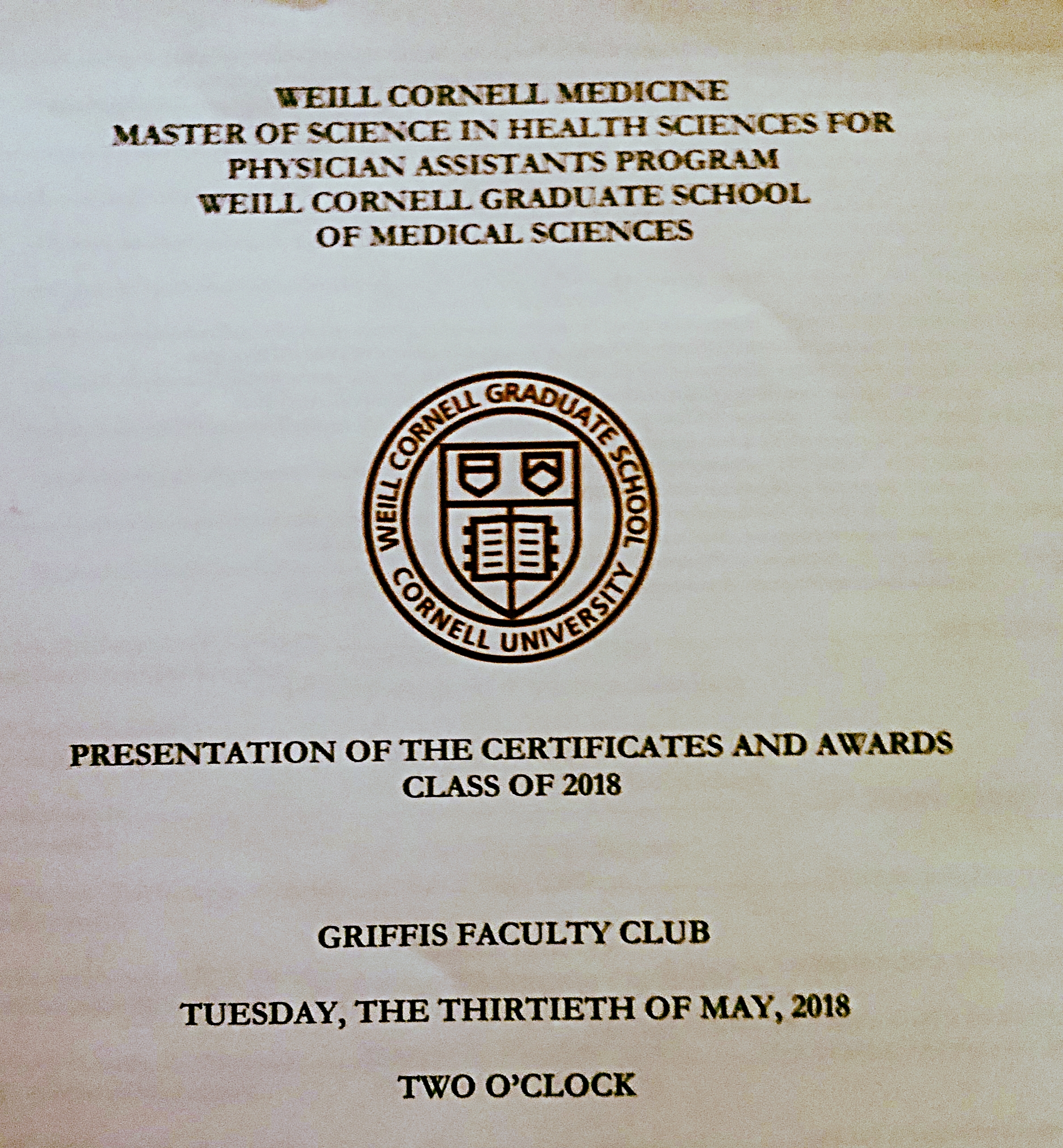
In 2010, my classmates at the Weill Cornell PA program gave me the privilege of speaking at our Certificate and Awards Ceremony for graduation. I am honored that eight years later, I was invited invited back as guest speaker by the Program Faculty to address this year's graduating class of 2018 on May 30th. Much of what I said during my first speech holds true today.
Program faculty honored me with an induction into Pi Alpha - The National Honor Society for Physician Assistants for contribution and service to our Profession.
It was a wonderful end to celebrate Brain Tumor Awareness Month and four years on May 13th since having brain tumor surgery and starting this humbling journey of recovery. Grateful to have been joined by friend/sister and 2010 alumnus Christina Pratt.
Dear Faculty and distinguished guests, I am honored to have the opportunity to address the graduating class of 2018. I’d like to start with one of my favorite quotes:
“Nothing in the world is worth having or worth doing unless it means effort, pain, difficulty…I have never in my life envied a human being who led an easy life. I have envied a great many people who led difficult lives and led them well.”
This quote was made by a man who was a military leader, governor, and the 26th President of the United States of America, Theodore Roosevelt. This quote should resonate with many of you as you look back and consider the amazing achievements you have made here. Remember the struggles, sacrifices, and promises you made yourself a little over two years ago. Think back to that first day you met your peers and observed them as they stood bravely and introduced themselves. You made mental notes of where they came from, what they accomplished before coming to PA school, and what inspired them to want to become PAs. Two years later, think about the journey you have taken since, the difficult and joyous times you have faced, and the bonds you have made together. Today dear graduates, we celebrate this friendship and we celebrate this beautiful journey.
Don’t let the smiling faces today fool you though. This journey has been long and has been difficult at times, forcing you to question your strength, competency, motivation, faith, and devotion. For many of you, it was difficult to be far from those you love and far from the comforts of a previous life. However, you soon found a surrogate family within your program. Today, as you collect your diplomas, these impressive certificates capturing in few words the awesome achievements you have made during your time here, please remember, that there has been so much you have gained in life in addition to what you gained in the classroom. So much that you have learned through friendships, relationships, and chance encounters.
In addition to all you have learned, I too would like to share with you some wisdom I have gained through my personal experience. I was a caregiver during PA school for my mother when she was diagnosed with AML and who ultimately succumbed to her illness. After a short leave, I returned and completed my degree and became a PA.
In 2014, after having only practiced a few years as a surgical PA, I underwent an elective procedure to have a benign brain tumor removed. Initially, I was expecting to discharge and return home a few days after surgery, but instead, became completely paralyzed on my entire right side and unable to identify one half of my body. I was 32 years old.
I was transferred to a rehab facility where after the eventual and painful realization that the landscape of my life had completely changed, I underwent aggressive physical, occupational, and speech therapy to establish what is now my new normal.
From my experience, I have learned that life does not always go according to our plans. It can change suddenly and sometimes drastically. Often, the thing we expect the least to occur is exactly the thing that does and that we find it is that very thing, that we need the most, to change who we are and to change how we appreciate what we have been blessed to have and will have in the future.
My experience as a brain tumor survivor is not unique in that I am an ordinary person who has been humbled by extraordinary circumstances. However, my perspective of this experience is unique as a Physician Assistant. Many of the things that I found most troubling were things I ordered for my own patients consistently and never thought twice about simply because either patients never complained or sometimes I was just too busy. For example, too busy to remember to cancel the order for finger sticks for a non-diabetic patient transferred from the ICU… BUT I REMEMBERED when it was my fingers that were stuck needlessly. Talk about karma. To say that I have been humbled would be an understatement.
Although knowing that there is always uncertainty can be at times unsettling it should not however; prevent us from dreaming and planning for the future. If nothing else, this sense of hope and determination allows us to have something to look forward to, the next day and for the rest of our lives. Whilst in rehab, once I could read and comprehend my phone texts, naturally I decided it was time to apply for a job, …completely discounting the fact that I was still paralyzed and a three person assist for basic functions. I stayed up late one night and the nurse found me finalizing my application for an academic position that I had my heart set on at the University of Bridgeport PA program. After inquiring why I was up late I said very matter of fact, “I’m just submitting my application for a job.” Stunned, she only replied, “I see”, and left.
The next morning, I was somewhat reprimanded by medical staff and counseled to see my new disability and recovery as a vacation. I was told that it would be unlikely I could return to work for a few years at least. After they left my room I felt disheartened and disappointed by the thought of functioning as anything but a PA and considered their suggestion. Unable to accept their bleak perspective, I instead answered enthusiastically when UB called me for an interview that same afternoon. After explaining my situation I was encouraged to call back when physically ready and told that my interview spot would be held if still available. It gave me hope and five months later when I was finally walking independently in my driveway, I interviewed and was hired two days later.
Today I am the Academic Director for the University of Bridgeport PA Program. Since surgery, I have also returned to clinical practice in Addiction Medicine, providing primary care for patients undergoing detoxification. My disability gives me A LOT of street credibility with my patients as it serves as a reminder to them, that we are all recovering from something.
My commitment to patient care and patient advocacy extends beyond clinical practice in that I am a volunteer for the American Brain Tumor Association, an Ambassador for the Connecticut Brain Tumor Alliance and recently, elected as a member of the Board of Directors. One of the best backhanded compliments I have received since my surgery is, “for a disabled person, you sure do a lot.”
I share this not only to highlight how amazing I am, because well I am, but also, so that you can be conscious of your own vulnerability to change and be sensitive to that same vulnerability in the lives of your patients and the lives of their loved ones. Remember that compassion cannot be taught just by words alone, it is a quality that is appreciated in others and developed and fine-tuned within us. As a patient, I experienced firsthand how crippling fear and doubt can be in dampening one’s spirits. So, don’t doubt your patients, you’d be surprised how far someone will go to regain some semblance of normalcy and to accomplish great things simply because they believe they can. With that said, don’t doubt yourself. You’d be surprised what you can accomplish because you believe you can. And like L’Oréal says, because YOU’RE WORTH IT!
Famous words attributed to JM Barrie about compassion, which have resonated with me for the past twelve years as a caregiver, clinician, and survivor are, “Be kinder than necessary, for EVERYONE you meet is fighting some kind of battle”.
Along with compassion, one must also be in constant appreciation of the various blessings we have in our lives. As an alumnus from this amazing institution, I too join you in your celebration of success at Cornell. With all that we have gained from our time at Cornell, we will always remember to give thanks to those who have given their time for our benefit. We give thanks to those who have been forthcoming with knowledge it has taken them years to acquire, but only a few weeks each, for us to absorb the superficial details. We give thanks to those who have allowed for extra time in their busy day so that we may have additional time to practice our clinical skills. We give thanks to the patients and their loved ones, who did not fear our short white coats, who did not fear our beads of perspiration, and for those patients who did not hesitate to be the guinea pigs as we made our first attempts.
Ralph Waldo Emerson once wrote,
“I cannot remember the books I’ve read any more than the meals I have eaten; even so, they have made me.”
As you complete your transition into the next phase of your professional careers, think back to your program and remember how blessed you were to have had the opportunity to attend such a prestigious institution. Be proud of your status as a graduate from one of only two Ivy League PA programs in the country. You were amongst the elite few who were chosen to be a part of the Class of 2018 at Cornell.
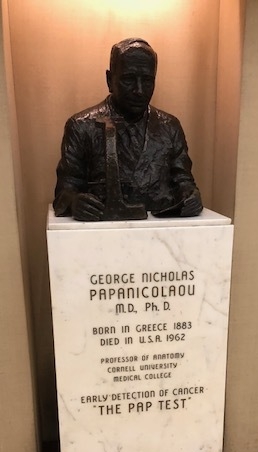
Give thanks to your program faculty for providing you with their guidance and support. Thank them for opening doors to institutions such as NYP Columbia, Cornell, Queens, to Memorial Sloan Kettering, and to HSS. These institutions, which are held in high esteem the world over, welcomed you and allowed you to be taken under the wings of some of the world’s most brilliant minds. What a privilege it has been not only academically, but from a personal experience as well to shadow clinicians who are considered pioneers in their respective specialties.
And now graduates, distinguished guests, and to the members of the Cornell community, I conclude my time here with you today. Graduates, let me again congratulate you and remind to feel proud of what you have achieved. Take with you the awe and respect for the human body and its many conditions and continue to seek knowledge even as you practice.
Think fondly of your alma mater, it has made you the competent clinician you are today. With that, remember always the strength and determination with which you achieved success in a difficult and challenging program and let that prevent you from doubting your ability in the future. With that, do not doubt your patients either, as they will continue to amaze you when you least expect it with their perseverance, faith, and perhaps good fortune. Be sensitive to the disposition and vulnerability in the lives of your patients and their loved ones. It is what differentiates a good clinician from one that is merely present.
As you don your long white coats and embark into clinical practice, remember that it carries with it a beautiful privilege coupled with tremendous responsibility. I know you will love being a PA and will contribute to the profession greatly. Lastly, remember to be kind, be humble, and be compassionate.
All the best. God bless. THANK YOU









@WeillCornell @UBridgeport @theABTA @CTBTA @AAPA
Returning to Clinical Practice After Brain Surgery
I remember him waiting patiently as I shifted nervously in my chair. He had just presented me with a golden opportunity, yet I hesitated. Looking down at his feet, I was avoiding eye contact, hoping to hide my anxiety. I contemplated his offer, wanting desperately to find the courage to accept. Only two years prior, I naively sought this very opportunity, ignoring the obstacles that were in my way after I underwent a surgical procedure to remove a benign brain tumor. After that surgery, I expected to return home and recover followed by my eventual return to clinical practice. Instead, I became paralyzed and was admitted into rehab and thus beginning my journey of recovery. Despite the significant deficit I experienced from paralysis, I considered multiple job opportunities for physician assistants, my profession and passion. I could not fathom departing from clinical practice, despite being told that I could not work with patients for at least two years after suffering what the physician at rehab described as a traumatic brain injury.
Yet that day, two years later, while I was walking with an assistive device, driving, and already employed full-time in academia, I was afraid. Afraid that maybe I wasn’t ready or good enough to provide patient care. The man that waited patiently for me to consider his offer was my employer, Dr. Daniel Cervonka, the Program Director for the Physician Assistant program with which I was employed. In addition to his administrative responsibilities at the program, Dr. Cervonka was also the lead PA for a drug and alcohol rehabilitation program, Recovery Network of Programs (RNP), which was seeking PAs at that time. Eventually, with his persistent yet gentle encouragement, I decided to take the offer.
In so many ways, brain surgery has changed the landscape of my life. I feel stronger as an individual knowing that I am able to overcome such an obstacle yet weaker because I am now far more susceptible to the devastating effects of fatigue and stress that many healthcare professionals battle on a regular basis. I am more empathetic having been on the other side of the white coat, experiencing anxiety regarding one’s diagnosis and prognosis, and frustration with the lack of communication or what I as the patient deemed inadequate time spent with a health care provider during my patient encounter. I took these valuable experiences with me, nervous with anticipation yet excited with hope. A stethoscope in one hand and an ID badge in another, I entered the clinic and started a new chapter one year ago, exactly two years after my surgery as the doctor had advised.
At first, I was slow, very slow. I fatigued easily carrying patient charts from one end of the hall to the other. Patients lined in the hallway, waiting to be seen by the nurses would shoot puzzled glances at the woman walking down the hallway with a cane in one hand and patient charts in another. The walk down was exhausting and embarrassing. After two years, I still struggled with a new identity of being “disabled”. In between patient encounters, I would rest my legs and my hand. We were still paper charting in the beginning and of all things fatiguing, writing was my nemesis. The physical exams were done without hesitation or difficulty. I had mastered my own technique and by following a regimen of head to toe, I developed a routine. After my first day I felt invigorated, thoroughly satiated by the experience. The fatigue both mentally and physically, would rear its ugly head the next day. I realized soon that I would need to space my shifts to accommodate my disability. After a while, I realized that I could also ask for help with carrying charts or calling on patients. Often, counselors would help in these areas or patient techs and I began to rely on them. This greatly minimized fatigue and helped speed up patient flow.
Interestingly, patients too are helpful and empathetic. These patients are undergoing detoxification from substances ranging from alcohol, opiates, to benzos and despite their own struggles, they never cease to amaze me with their concern for my well-being. These are underserved and underestimated individuals, many of whom grew up in and out of prison, suffered exploitation, years of physical and sexual violence and yet, when they see me, they are concerned for my health. Curious, they will stop me in the hallway to ask about my disability and how it came to be. I distinctly remember earlier on, one particular patient, emaciated and weathered by years of battling a heroin addiction and poor nutrition, appearing far older than “their” 50 or so years of life who was genuinely concerned about me. Seated in the hallway seeking comfort in solace, as many patients do, “they” rose to their feet as I was passing by and gently grabbed my arm . “Honey, what happened to you? How come you have a cane?” Caught off-guard, I hesitated. How much I should share, I wondered. Should I even share? Eventually, I thought, maybe it will help “them” see that there are struggles we can overcome.
Unsure, I responded, “I had surgery for a brain tumor and became paralyzed. As you can see, I’m still recovering, but have come very far.”
“Honey, I’m going to pray for you. I’m so sorry, too young for that. God bless you. That’s amazing.”
I remember feeling stunned by this response as I was not expecting such kindness. If anything I thought it would satisfy “their” curiosity. A few others had gathered and also echoed their prayers and well wishes. I looked around at their sympathetic smiles, overwhelmed by their acknowledgement.
“I guess we’re all recovering from something” I said. I remember this statement striking a chord with them. I realized too the power of what I had just said. It was true, in life, we are all recovering from something. I stood there in the hallway with them for that brief moment not only as the clinician, but as a patient myself. One of my favorite quotes comes to mind as I often remember that moment, “Be kinder than necessary, for everyone you meet is fighting some kind of battle.”
Since my return to clinical practice, I have successfully recertified my boards this fall and have been able to share my many patient care experiences with my students, in hopes that all the things I am blessed to have experienced can one day guide them into becoming more sympathetic and well-rounded clinicians. After practicing again, I feel validated teaching young aspiring PAs the values I hold dear in regards to patient care and also, I feel complete. For two years, something was missing, something which I only found upon returning to clinical practice. As I continue to grow in my profession, benefiting from the help and support of my colleagues, I make sure to remember to take each step down that hallway and in life, one step at a time or as we say in medicine, “all things in moderation”.
Return to clinical practice after Brain Surgery
Today, with a book-bag and stethoscope, I returned to clinical practice for the first time in a little over two years since my brain tumor surgery. For the joy and confidence in seeing patients and working with other healthcare professionals, I am forever grateful for friend and mentor, Dr Daniel Cervonka. For anyone thinking of returning to work at any point in recovery, find what makes you happy but that which fits into your "new normal".
#braintumorawareness
#BTA
#physicianassistant
Seeing Stars & Other Signs of Pain in Recovery & Hemiparesis
About two years ago, I assumed that the brief use of narcotics in the post-operative period would be the extent of my experience and management of pain; however, I have been proven wrong, repeatedly. I assumed my small incision would produce minimal pain, well, until it didn’t.
Initially post-operatively I was well taken care of. The transition of relative comfort to pain happened approximately two weeks later when I first experienced spasticity. I remember mistaking the involuntary movement in my arms and legs as return of function, but learned that it was not, at least not entirely. According to StrokeSmart.org, as a result of an injury to a normal functioning part of the brain, “Spasticity is tight, stiff muscles that make movement, especially of the arms or legs, difficult or uncontrollable.” For two days I went from a compliant and pleasant patient to one that was inconsolable, miserable, and uninterested in PT. My legs felt like a wet towel that was repeatedly wrung out. The nurses were angels who would manually massage my legs to help alleviate the pain. I was started on Valium and Gabapentin (Neurontin) and given Ambien to help sleep at night. Once the Gabapentin levels created the desired effect, others were discontinued, thank God because Valium was horrible.
The months that followed were relatively pain free aside from the soreness of wearing a leg brace or resting my arm on an unkind surface for prolonged periods of time. My paralysis was improving and by mid-September I had begun walking independently in my driveway, enjoying the crisp autumn air. My recovery followed the pattern noted in reduction of brain swelling evident on serial MRIs (every three months the first year). By December, I became aware of movement in my right shoulder and this was the first time I experienced pain since my Valium experience in rehab. The pain was excruciating and I found myself unable to use my right upper extremity effectively or at all, instead elevating it and carrying it like the Hunchback of Notre Dame. Naturally my elder brothers in their usual supportive fashion found an opportunity to poke fun at my inability to move my right arm often mimicking its stiffness in conversation. Eh, I thought it was funny too, but I also enjoy self-depreciative humor. This started my eight months of exclusive right shoulder occupational therapy treatments after which I was advised to seek other care as the focus was limiting improvement on other areas of need such as my hand.
I found myself walking into a Naturopathic clinic at the University of Bridgeport. Being one of the coordinators for our graduate Integrative Medicine Course, I kept an open mind. I had friends who swore by acupuncture, so I figured why not. I found acupuncture to be very effective, but extremely painful, which I expected from Eastern Medicine. I noted some improvement in pain, though not completely and not long-term. The intensity of the treatment often resulted in fevers and soreness for two to three days with one day of bliss followed by return of symptoms usually by the time I was due for another treatment. This was a cycle for a few months.
Despite pain in my shoulder, I returned to the gym at RetroFitness in North Haven, CT. Wanting to lose weight and strengthen my body, hoping it would help with issues I have with balance, I found myself going six to seven days a week. Between acupuncture and the gym, I felt I could tolerate the pain and that I was at least trying my best to manage. Unfortunately in December, I started experiencing incredible pain in my left leg, “the good leg”. I awoke one morning to find a red, angry, swollen knee. I remember rolling my eyes and feeling annoyed, I wanted so desperately to ignore it. I felt like Kimberly “Sweet Brown” Wilkins, “ain’t nobody got time for that”. Alas, fearing immobility would affect my ability to drive, I scheduled an appointment with my primary care physician who got me a consult with a Yale orthopedic surgeon stat. After x-rays and an MRI, I was told I had evidence of osteonecrosis, likely from exposure to steroids around the time of surgery. To make matters worse, I fell in the comfort of my home, sustaining an injury that for the lack of a better expression, made me “see stars”. It took me 15 minutes to get off the floor and the next morning I was completely unable to move my right shoulder. It was a devastating blow to my ego and self-confidence. I was referred to Dr. Patrick Ruwe of CT Orthopedic Specialists, who examined my shoulder and leg and said you don’t need bed rest or a knee replacement, you need therapy. So there started my journey with STAR therapy in Hamden, CT where I continue today. I placed my gym membership on temporary hold and workout aggressively at rehab with their amazing team of therapists. It is not without pain, from manual manipulation of trigger points and a rolling pin like contraption for IT Band Syndrome pain, but seeing stars that will result in long-term relief is worth it. I just say to myself, “no pain, no gain”.
This past month I walked two blocks at work for the first time and it felt great to rely on my leg again. To be independent. To feel strong again.
In addition to my shoulder and leg pain, this past month I have started experiencing terrible headaches originating from the incision site. At first I attributed the pain to normal stressors such as work or social obligations; however, the pain progressed from headache to nauseating and debilitating. It often feels like I sustained a recent injury to the incision site. After speaking with my neurosurgeon I was told that post-craniotomy pain was common and again was advised to try acupuncture as there has been relief noted by neurosurgery patients.
This past Friday, I had my recent MRI and was told it was “clean”. I felt such relief, actually blessed. I have now officially graduated my second year since surgery and will only require annual MRI exams instead of every 3 months or six months. I have accepted pain will always be present to some degree or another but that I will have to be more creative in my management.
After all, the show must go on.
One year work anniversary
Blessed to celebrate my 1 year anniversary today. Four seasons of growth, laughs, and support by an amazing group of colleagues and students. As I sit here with my colleagues enjoying tearful laughs, I think of last year and I am grateful I took the chance and applied. One of my favorite quotes my cousin shared with me, 'If your dreams do not scare you, they are not big enough.'
Now that you’ve been referred, here’s how you can prepare for your consultation with a specialist:
1. Prepare a Folder or a binder with your medical records:
I did this for my mother when I was her caretaker and it reduced her anxiety and stress as well as that of my own. I organized the binder with tabs labeled as: Provider Info, Patient History, Directions but you can organize per your preference.
Provider Info: I listed the physician’s name, number, location, and specialty. Be sure to include your primary care physician and/ or any referring physician. I also listed social workers and clinical care coordinators who facilitated my mother's care and discharge. Home Health Aide agencies, medical supply companies, etc.
Patient History: I photocopied my mother’s insurance card and kept a copy in the binder as well as a copy of her driver’s license. I then included a Word Document with notes regarding her MD/ Hospital/ Homecare Visits as well as all documentation they provided.
Directions: To various sites we would visit.
Please use caution as sensitive information must be safeguarded. I kept the binder with me at all times unless my brother or other family member I trusted was assuming duties.
2. Keep a list of current Medications:
Medication bottle themed ID card that I picked up at during a recent visit to rehab. It's cute, compact, and perfect for anyone to keep with them.
This includes those that are prescribed to you as well as anything herbal and over the counter. You can add this list to the binder as well as keep a fold out mini medication card in your purse or wallet. Ask your MD’s office for one, most will have one readily available for patients to fill out and use. You can include pictures of the pills prescribed to distinguish by appearance.
Here are some sample tables I made:
3. Bring any CD’s or images with you.
In some cases, the physician to whom you are referred will have you complete certain diagnostic tests prior to your consultation. Depending on their access to the testing facility, you may have to bring a CD/copy of the test results with you. Sometimes you will be given a copy at the time of the visit, other times you will need to request a copy from the Medical Records Office. I had a neurosurgical consultation with an MD in New York and brought my MRI CD with me so that he could make his assessment. Don't rely on the referring physician to fax or mail them, it could delay your appointment.
4. Avoid “Google” and the act of self-diagnosing.
Did I listen to that advice? No, of course not. But I wouldn’t be a true advocate or PA if I didn’t at least tell you not to. Yes, it is reasonable and expected to be curious, but don’t assume that you have everything you are reading about. Often, you can spend (waste) valuable time with the clinician discussing hypothetical situations instead of addressing key findings/ indicators, a list of differentials (possible diagnoses based on findings/ clinical presentation), and treatment options or future outlook. DO however, google specialists involved in the general area of the problem, if known. You MUST do your due diligence and be your own advocate or one for someone you love if you are a caretaker. Educate yourself on providers who are known for the “problem” you are seeking help for. There are organizations which can help guide you. I've listed a few for brain tumor patients and cancer patients on my Resources page.
5. Bring a tape recorder with you (especially for those with phones not equipped with one).
Ideally, you can bring a friend or family member with you. Often, hearing words like “tumor, lesion, cancer, surgery, stroke, etc.” are enough to shock anyone, and not remembering key details of the visit is frustrating and frightening. Sometimes with my own patients, I would find they wouldn't tell me if they didn't understand something out of fear of embarrassing themselves or appearing unintelligent. I had a background in medical sciences so I was able to be a crutch for my mother but even I found some jargon to be beyond my comprehension at that time and would do additional reading to learn. Then, I was fortunate in that two of my dear and close friends went with me to my consultations separately and they were both in the medical field, but not everyone has that luxury. Ask the physician if they wouldn’t mind you recording the conversation and review the file aftewards.
6. Asking Questions
My first time writing (left hand), 2 months after surgery. Part of preparation for my first follow-up visit with Dr. Diluna.
A clinician should be understanding and compassionate to what you are feeling and having to deal with. Don’t feel nervous to ask a question, it is your RIGHT. Ask what their experience is with your particular situation. Ask if anyone else in the practice also performs/ treats these conditions. (You should google them too)
The American Brain Tumor Association (#theABTA) shared an amazing list of questions to keep with you for your appointment and I would strongly encourage you to look at them or share them with someone you know visiting with a specialist.
http://www.abta.org/resources/care-and-treatment-section-resources/questions-for-health-care.pdf
7. If you’re specialist recommends surgery:
Regardless of the type of surgery and reason, basic questions applicable to all are what is the “usual” amount of time for duration of surgery? What imaging or testing will I need prior to surgery? What is the expected recovery time immediately post-op and when are patients discharged home typically? How often will I require follow-up care or visits with you?
For those with a tumor: You will likely be given information regarding location, size, quality or appearance on imaging, etc. Additional questions to consider include: What is the rate of recurrence? What are contributing factors which increase the likelihood of recurrence (genetics, previous recurrence, exposure, etc.)? Will I need chemotherapy or radiation (even if prophylactically)?
8. Don’t be afraid to ask for a referral if you would like a second opinion.
You should never be uncomfortable or hesitant to seek a second, third (etc.) opinion, unless you are comfortable with the first, and only you can judge that. As a patient, when my surgeon suggested I consult with a surgeon in NYC, I felt comfortable with him and appreciated his willingness to recommend someone. And yes, I did seek another opinion from the neurosurgeon he recommended. How many should you have? Too many sources can be overwhelming and counterproductive. Only you can gauge how much is enough, but use caution. Spend your time and energy wisely. For me I needed it for my ongoing recovery after surgery.
9. Update your provider visit information in the binder after your consultation.
Jot down key points from your appointment. It makes a great reference and no second guessing, ‘wait, did she say this was the next step?’, ‘what did he want me to do?’ It can be overwhelming, and for me it was. But, you figure out shortcuts, a rhythm, and slowly you feel like this (organization) is one thing right now you can control.
10. Lastly, keep a positive and proactive outlook and try to have a sense of humor despite the craziness.
As insane as this may seem, even when you are dealing with the worst, laughing can be therapeutic. It may not happen at first. It certainly didn’t for me but by my third appointment I was past the disbelief, emotional stage and in tune with my personality, I got to the acceptance and proactive stage. At one particular visit, I remember sharing with my MD and a mutual friend, also a physician that I read some patients develop serious personality disorders even becoming promiscuous after neurosurgery. Having lived a fairly conservative life, I stated I thought promiscuity would be preferable over death or neurocognitive decline. Luckily, since my surgery I’ve not suffered from death, neurocognitive decline, or the development of a loose character.
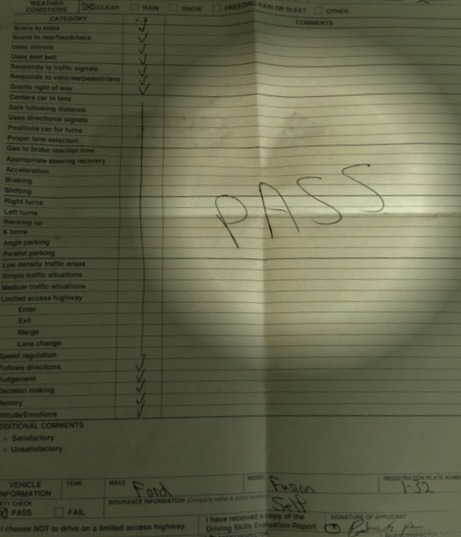
Driving After Disability IS Possible!
Driving after disability IS possible! It's taken me a year to finally sit behind the wheel for the first time for my driving eval and I passed! If you or someone you know is dealing with this then please visit the link below on ways to get started.
Yes, I can and I did.
Watch out! Here I come...
10 Things I learned after having Brain Tumor Surgery, as a Clinician & as a Patient
10. Surprisingly, it’s the relatively “small stuff” that you remember as making you the MOST MISERABLE.
Although I’ve had neurosurgery, spent hours cumulatively lying in an MRI machine, developed paralysis of my dominant side, and have been involved in extensive rehab therapy, I surprisingly did not and do not find these to be the worst things about my experience. In fact, I wasn’t aware of anything during surgery obviously thanks to amazing drugs coupled with an equally amazing anesthesiologist and this feeling of being in a dream like state lasted a few weeks after as well. As for MRIs, they can become tolerable by simply asking for a mirror to be placed inside to give the illusion of extra space. Trust me this helps a lot.
Interestingly, the things which I found to make me the most miserable are also the least invasive and obvious in comparison to other more harrowing events. First, having a suppository. Now keep in mind, I was completely paralyzed on my right side. Inducing a bowel movement in someone who can’t move is inhumane. Next, straight catheterization. This was by far one of the most uncomfortable and excruciating things my foggy brain retained in memory as a fresh post-operative patient. At one point, I begged the nurse to demand the fellow to order me a foley since a UTI was the LAST worry on my jetlagged mind. Equally as horrible are glucose finger sticks to test for blood sugar levels. My fingers went numb on my left side to match my already numb right hand. Luckily this was discontinued when the steroids were.
Lastly, my next offender is the Lovenox injection (blood thinner). These were the bane of my rehab existence. They are given once daily, under the skin (subcutaneously), usually where one has the most fat accumulated. In my instance, it could have been anywhere, but we opted for the belly. The injection site BURNs for up to five minutes after administering and it was so bad that the only way I could entertain myself was to play “Happy” by Pharrell and laugh because I felt anything but.
The best part about all of this is that all of the items I have mentioned are those which I have ordered for my own patients as a clinician. To experience them myself, gave me a whole new appreciation of what my surgical patients endured. Karma, enough said.
9. You forget many of the people you have met in the hospital.
Although unfortunate, you might forget names and faces of people who helped you in your time of greatest need. Luckily, I know I thanked them. Actually, I even offered them my food and drinks. I was so high on meds, I probably would have offered my kidney if asked but luckily I wasn't. My family and friends tell me I was the nicest patient they have ever met. Thank God since as a clinician I would often joke with colleagues that I never wanted to be that crazy combative or verbally abusive patient one would sometimes encounter. It can happen to anyone so if it was you no shame, we (clinicians) don't hold grudges. I digress, but I have always have been one of those people who goes out of her way to introduce myself and become acquainted with others who I encounter, in whatever capacity. I’m a little embarrassed, and yes I realize given the circumstances it happens, but I don’t remember the names of some people who cared for me post-operatively and earlier on in rehab, regardless of how amazing.
8. Laughter truly is the best therapy.
Image obtained via Pixbay (no attribution required).
I have taken a variety of medications since my surgery at various points postoperatively, but nothing can make you feel as good as a big dose of laughter. Multiple doses to be exact, and no you can never overdose. I think it was in rehab when I first laughed and I just remember letting go completely. It felt like a fresh breeze. I loved to laugh with my nurses, PCAs, techs, and therapists. I had this routine where when I was being returned to my room from therapy, being that my room was the closest to the nurses station, I would burst out in a Salt ‘n Peppa verse. “Salt n Pepa’s here, and we’re in effect”. The nurse on duty that day would respond, “Want you to push it back”. With everyone then chiming in the chorus, “ooh baby baby, ooh baby baby’. Laughter literally was one of the most important things that influenced my recovery as humor is a big part of who I am. It helped me take care of my mother when she was diagnosed with leukemia, my patients when I worked clinically, and it helps me today as I have dealt with and currently face the uncertainty of anything surrounding my brain tumor experience.
7. Follow-up MRI’s and doctor visits can be a scary thing.
May 13th 2015 will be my one year anniversary and as of yet my MRI has been negative. The first year after surgery the monitoring is every three months and now I can progress to every six months. Although the results have been negative, I still get just a little worried every time I go in to see Dr. Diluna. Just that brief moment as he walks into the exam room door I think, “what if there is a recurrence”? Then all of the possibilities run through your mind and you think, I just never want to have surgery again and I think anyone that has undergone this can agree. I am grateful that there are measures today which can be taken to eradicate patients of disease; however, once is ideal, and even that really is too much.
6. Even after major life altering events, eventually you find yourself worrying about the same things you worried about before.
Initially after my surgery, I was on a high, and no I am not referring to the feeling of euphoria induced by narcotics. I am referring to the feeling of extreme gratitude for being alive and in my instance for being neurocognitively intact. Prior to surgery, I told Dr. Diluna, all I want is to wake up the same person. So after surgery, I was ecstatic that despite the fact I couldn’t walk or move my arm or leg, I could still tell jokes, no matter how corny. And if you’re wondering why I didn’t sit in my room at rehab everyday crying all the time, it’s because I’m a glass half full kind of woman and this has served me well. But even with all the gratitude, after the initial first month of being in rehab, I found myself worrying about the same things I worried about before surgery.
My student loans (I owe what most people pay for a mortgage), cell phone charges, car payment, car insurance, the list goes on. Luckily, I had savings, not tons but enough for a few months. It’s scary since I knew it couldn’t last me forever and not being employed at the time I worried about that too. My advice, get as much of your life figured out as you can before being diagnosed with a brain tumor and good luck with that.
Vanity was another thing I never thought would seem important anymore, but as Maury Povich would say, “the lie detector test revealed, that too was a lie”. After losing most of my hair from the stress of surgery and steroids, I saved and bought hair extensions once employed. Necessity? No, but feeling good about yourself affects your ability to perform optimally both socially and professionally.
5. Food and everything that once had flavor, no longer tastes that way after surgery, at least for a while.
Image obtained via Pixbay (no attribution required).
I knew that patients could develop "metal mouth" or an altered sense of taste as a result of medications as it happened to my patients and my own mother as well from chemotherapy, but I was not expecting this oddly enough, for myself. I was completely blindsided when I drank my favorite poison, Diet Coke, and I almost wanted to vomit. I just remember it tasting awful and thinking my brother got me a dirty cup or some crazy flavor like root beer. The interesting part is the only food that tasted good was the food at the cafeteria and takeout Chinese. This lasted even when I was discharged home for about two months. A total of about four months after my surgery my taste started normalizing. Until then I would have cravings but once the food arrived or was prepared I couldn’t stomach the thought of eating it.
4. Pain medicine can result in very serious nightmares.
Image obtained via Pixbay (no attribution required).
Even as I type this, I can’t help but imagine a commercial voice quickly reading this as side effect in one of those pharmaceutical ads. At first I had some intense nightmares while I was in rehab due to the narcotics and steroids and eventually, I opted on just taking Tylenol, which also helped eliminate the need for any evil suppositories. Often, I would wake up from dreaming that a dark shadow was running around in my room or my craziest dream that I was sleeping in my bed in a conference room while my former colleagues were having a meeting. That for some reason was the most disturbing as I kept thinking I’m not dressed or prepared! I had to sleep with the door open for the remainder of my time in rehab so I could hear the nurses station when I awoke at night. The nightmares stopped as I was weaned off the medications.
3. Even clinicians are non-compliant patients.
Image obtained via Pixbay (no attribution required).
To this day, almost a year later, I still struggle with compliance. When I see my neurosurgeon, primary care physician, or rehab internist I am always embarrassed to admit that I’m not always the most compliant with medications for spasticity. I actually had the audacity to ask my neurosurgeon to change my dose to once a day since TID (three times a day) was too difficult in between teaching classes. To which he smirked and gave me a mental, ‘are you freaking kidding me’ head nod. For those of you reading this that work in healthcare, a lot you know exactly what I’m talking about. Luckily not everyone, just think Dr. Oz and picture him having green tea and doing yoga. For me, I guess I can blame my mother who as an immigrant raising us in the 80’s would prophylactically give my two brothers and me children’s Robitussin even if only one of us was sick. Since she was gone all day for work, we’d each get all three doses for the day in the morning. My mom mentioned this ingenious trick she figured out to our pediatrician who kindly informed her this was not prophylaxis but dangerous and yes, she promptly stopped. Needless to say, I probably developed a bad once a day habit very young.
2. You should never doubt your patients.
As a clinician I sometimes I failed to see potential in complicated peri-operative patients . It was miracles that made you stop and take a moment to appreciate a greater intervention, beyond medicine, which saved patients. I've seen patients who came in practically lifeless but would walk out a few months later, a little bruised of course, but alive and grateful. Still, it wasn't until I became a patient and met others who were admitted to the stroke unit with me that I realized you just never know how much patients can amaze you. How much they can push themselves to reclaim some of the glory of a healthier, previous life.
1. You should never doubt yourself.
Before my surgery, I saw a job posting for an academic positon and I thought I’ll be home a few days after surgery, I’ll apply when I have recovered afterwards. I had no idea I would develop paralysis and go to rehab. Even in rehab, much to the dismay of my physicians and nurses, I wrote my cover letter, granted it took me a lot longer than normal, and I submitted it. I was called the next day to schedule an interview but given my physical condition and at that point neurocognitive fogginess, I was not able to interview until 5 months later and was hired. It could have been very different for me had I not applied. I was told gently but repeatedly by my medical team and some family and friends to take it easy this year, apply for diasbility and just focus on recovering but I'm glad that at a point in my life where I was my weakest both physically and neurocognitively, I took this chance despite the great risk of being rejected. Now, when I speak about my experience with my students who are aspiring clinicians at the University of Bridgeport Physician Assistant Program, I make sure to tell them to never doubt their patients. I tell them, you will be surprised how far someone is willing to go to have something they think about night and day. I read the job description literally every day and it motivated me to work harder in rehab and continue to practice walking until I could walk into my interview. I saw my physiatrist after I was hired and she was in tears and stated she used to feel bad for me when I was inpatient because I was so passionate about teaching at UB and she didn’t think I would be physically able to.
Ultimately from my experience, I have learned my greatest and most difficult lesson to never doubt myself as I will have many opportunities to appreciate how far I can go to accomplish what others and sometimes even I myself have considered once impossible.